Common Dementia Behaviors: Expert Tips for Understanding and Coping

As many as 90% of people who have dementia behave in ways that challenge or worry their caregivers, according to research on dementia behaviors. For example, a person who has dementia may become more easily agitated or aggressive. Or, they may wander off and get lost in their confusion or during a bout of sleeplessness. These troubling dementia behaviors test caregivers to the core. If this sounds familiar, know that “you are not alone,” says Cleveland Clinic Center for Geriatric Medicine Section Chief Dr. Ardeshir Hashmi. Behaviors like aggression, confusion, sleep problems, and wandering are common, but they can be managed, Hashmi explains.
Let our care assessment guide you
Our free tool provides options, advice, and next steps based on your unique situation.
Key Takeaways
- Up to 90% of dementia patients experience behavioral changes. Confusion, aggression, sleep problems, and wandering are some of the most common behaviors.
- Many factors contribute to dementia-related behaviors. Some behaviors appear as dementia progresses, while others may be caused by frustrations or medications.
- Handling dementia behaviors can be tricky. Patience, understanding, and coping strategies can help greatly.
- You are not alone. As a caregiver, you can utilize respite care, and support groups, or explore memory care options to help you better cope.
The most common dementia behaviors in the elderly
“Dementia-related behaviors” is often used as an umbrella term to describe a group of behavioral symptoms associated with Alzheimer’s disease and other dementias. As dementia progresses, your loved one may start to show worrisome behaviors, however, many are common. In fact, up to 90% of dementia patients are affected by some of these common behaviors:[01,02,03]
- Confusion and repetition
- Aggression and agitation
- Sleep issues
- Disinhibition
- Wandering
- Hiding and hoarding things
If you notice any of these behaviors, be sure to discuss them with your loved one’s physician. It’s important to discuss all new symptoms to rule out or treat any medical conditions that could be causing the behavior, such as comorbid mental illness.
Below, you’ll learn more about how and why some of the most common dementia behaviors may manifest in your loved one. You’ll also get Dr. Hashmi’s advice on how best to handle them as a caregiver — for your sake as much as that of your loved one.
Dementia behavior: Confusion
Brain changes that occur with dementia can lead to confusion, often becoming more common as dementia progresses.
Common signs of confusion in a senior with dementia may include:
- Repeating the same questions or phrases over and over
- Not recognizing formerly familiar people or places
- Becoming disoriented
Caregivers who spend many hours with their loved one may hear phrases and answer questions on repeat: “I want to go home!” “This isn’t my house.” “When are we leaving?” “Why are we here?”
Common causes of dementia-related confusion
Like many dementia behaviors, confusion can have a number of triggers or root causes. Factors that may contribute to disorientation include the following:
- The environment. Is there too much noise or chaos occurring around them? Perhaps it’s too cluttered or crowded.
- Poor communication. Are people talking too fast around your loved one? Are they not providing enough time for your loved one to process? Are people presenting them with too much information at once?
- Lack of prompting and cueing. Family members or caregivers should be clear with verbal and physical cues. It can help a loved one with dementia stay on track when they don’t understand the situation in front of them.
- Sundown syndrome or delirium. Up to two-thirds of individuals with dementia experience an evening behavioral shift characterized by increased memory loss, agitation, confusion, and anger.[04] “It may not exactly happen at sundown, but there’s always this hour — the witching hour — where suddenly the same person may completely change,” Hashmi says.
- An unexpected change. Did your senior loved one just move to a new place? Did their routine change?
- Paranoia and hallucinations. Dementia leads to complex changes in the brain, which can result in delusion. Seniors may see things that aren’t really there, develop false beliefs, or become suspicious of caregivers and loved ones.
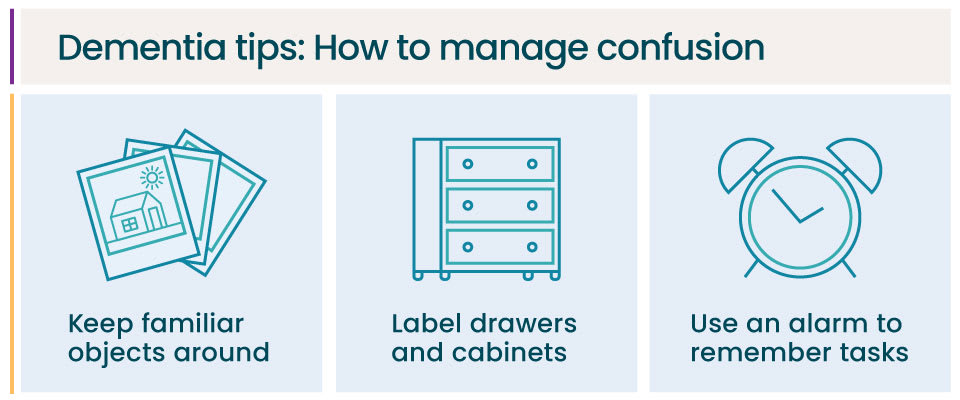
Tips for managing your loved one’s confusion
“Simplification is key here,” Hashmi says. To help minimize confusion, he suggests several ways to simplify both the home environment and your interactions:
Provide structure.
- Keep familiar objects around to help reorient your loved one.
- Label drawers and cabinets. This is especially helpful if confusion about where to find things is a common trigger.
- Use tools such as alarms, calendars, and to-do lists to help them remember tasks.
Deliberately use simple, short sentences and ask yes/no questions.
- Normalize their experience. Say, “This seems confusing, I agree. Let’s figure it out together.”
- Lead with what you think might be happening. For example: “It seems like you’re looking for something.”
- It’s often much easier for your loved one to answer yes or no questions, instead of coming up with the words themselves. “Are you looking for your keys? Are you looking for your glasses?”
Lastly, Hashmi says, it helps if you can learn to accept the confusion. In the moment, he says, whatever your loved one thinks is real is in fact their reality. For example, they might think they’re at work when they’re really at home. If that belief isn’t hurting them or anyone else, it’s OK for you to play along a little bit. Confronting or trying to change the belief often leads to agitation and aggression.
“For us as caregivers, we have to be OK with that confusion,” Hashmi says.
Read more:What Do Dementia Patients Think About?
Dementia behavior: Aggression
Verbal threats and physical aggression can be among the more serious dementia behaviors. These verbal or physical outbursts may occur seemingly out of nowhere. They tend to happen in the middle to later stage of dementia, when patients can’t communicate their needs.
One study found that aggression occurs in approximately half of dementia patients.[05]
“I hear very palpably how upsetting that is, how distraught they feel,” Hashmi says of caregivers. “They are trying to make sense of it — ‘Why me? I’m the one who’s here for you? Why are you angry at me? I’m trying to help.’”
Common causes of aggression
Aggression can stem from:
- Confusion. When a senior is feeling disoriented and scared, they may act out with aggression.
- Physical pain or another unmet need. When a senior can’t verbalize or address needs such as hunger, thirst, or pain, it’s common for frustration to build, Hashmi says.
- Frustration. A senior with dementia may become frustrated if they feel ignored, patronized, or treated as an imposition.
- Emotional pain. Sometimes, agitation can be a sign that someone with dementia feels lonely, depressed, or isolated.
- Discomfort with a specific task. Does aggression come out specifically at bath time, bedtime, or while your loved one is getting dressed? These tasks may be triggers for aggressive behavior.
- Reactions to medications. Has your loved one recently changed medications? Do they experience difficulties with medication management? This might be interfering with their dementia diagnosis, leading to aggression.
- Vision or hearing loss. Issues with vision or hearing can compound the typical disorientation of dementia and can cause seniors to act out in confusion or as a cry for help.
- Sundown syndrome. Does your loved one become aggressive around sunset in particular?
- Fear. People often are confrontational when approached or touched by someone they don’t know. For seniors with dementia, who may not recognize caregivers, doctors, and community residents, many daily interactions can alert a “fight or flight” response.

Tips for handling a senior’s aggression
Most importantly, try not to take the aggressive behavior personally, Hashmi says.
“The classic line I always use is that this is the disease talking. It is not the person,” Hashmi says. “There is a lack of awareness in that moment. It’s not your mom or dad or spouse saying that. It’s the disease.”
When you are faced with a loved one’s aggression, Hashmi suggests employing these 4 Rs:
- Reassure. It can be difficult to do in the moment, but start by reassuring your loved one. For example, Hashmi suggests you might say something like, “I’m here for you. I’m still here for you. It’s OK.”
- Reorient. If they are disoriented, reorient them to their environment and with a familiar object. Say, “Look, we’re at home. Here’s a picture we have.”
- Redirect. Redirect your senior toward a familiar object, anything that gives them joy and comfort. “It may be family photos, it may be a keepsake, it may be something that has great meaning and value to them,” Hashmi says. “It helps redirect and also helps reorient them.”
- Reminisce. Help them connect to a long-term memory. E.g., “Remember when Joe was born?”
Dementia specialists also recommend the following tips to handle aggression in individuals with dementia:
- Listen. Listen to their concern, restate it, and let them know you are on their side.
- Don’t argue. Instead, try to take the blame. Defuse the situation with an apology — “I’m sorry that happened” or “I’m sorry that upset you, I won’t do it again.”
- Try to find the cause. Realize that there is meaning behind their aggression. Try to assess their surroundings and see the situation through their eyes. In the future, try to avoid whatever you believe caused their aggression.
- Attempt a change of scenery. The environment may be causing the aggression. Changing rooms or going outside may help them calm down.
When they’re feeling calmer, Hashmi says, you can try asking yes/no questions to help determine whether an unmet need is causing the behavior. Ask: Are you hungry? Are you thirsty? Are you in pain? Are you tired?
Let our care assessment guide you
Our free tool provides options, advice, and next steps based on your unique situation.
Dementia behavior: Sleep problems
While quality sleep tends to decrease as you age, people who have dementia experience more sleep disturbances than other seniors. In fact, sleep problems affect up to half of seniors with dementia.[06]
Common sleep issues may include:
- Difficulty getting and staying asleep
- Agitation and restlessness when trying to sleep
- Thinking it’s daytime when it’s night, going as far as getting up, getting dressed, and wanting to start the day
- Excessive sleepiness during the day
Sleep disturbances are hard on patients and caregivers alike, Hashmi says. “It’s physically and mentally exhausting to be up night after night.”
Common causes of sleep problems in dementia patients
Troubled sleep is thought to be a dementia risk factor as well as a behavioral symptom. Here are some factors that may contribute to your loved one’s sleep problems:
- Brain changes. Dementia patients have steeper changes in their brain’s sleep architecture and their circadian rhythms, causing sleep disturbances.
- Over-the-counter medications. Some over-the-counter medications labeled “PM” can disrupt sleep by making patients sleep for a bit but then making them more confused or sleepy at the wrong time, Hashmi says.
- Diet. Caffeine, excess sugar (especially before bed), and alcohol can disrupt sleep patterns, Hashmi says.
- Electronic screens. The blue light from a computer, portable electronic devices, and television screens can delay sleep and disturb sleep patterns, Hashmi says.
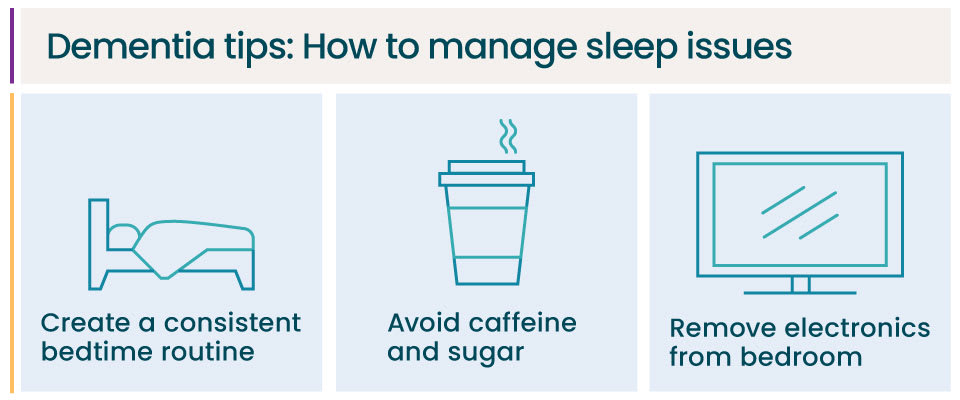
Tips to help manage dementia sleep problems
There are ways to help your loved one get a better night’s sleep, Hashmi says.
Avoid things that disrupt sleep.
- Limit caffeine, alcohol, and sugar near bedtime.
- Avoid over-the-counter sleep aids. Instead, Hashmi suggests you talk to a doctor about whether melatonin might help your loved one sleep.
- Remove electronics from the bedroom and/or use blue light-blocking glasses.
Create a routine that supports sleep.
- Make sure your loved one gets enough daytime light to help with circadian rhythms.
- Change into comfortable clothing, signaling nighttime.
- Consider warm milk, a hot shower, relaxing music, or reading before bed.
- Pick a bedtime — not too late — and stick with it every night.
Dementia behavior: Wandering
Sixty percent of people who have dementia will wander.[07] As their memory declines, they might leave a confusing situation or suddenly try to find someone and become disoriented and lost.
Such wandering can be dangerous, even life-threatening, yet caregivers often feel guilty for taking measures that will keep their loved one safe. The classic quandary that caregivers express is: “I don’t want my mom or dad or spouse to be a prisoner in their own home, and yet this is what I feel I’m doing,” Hashmi says.
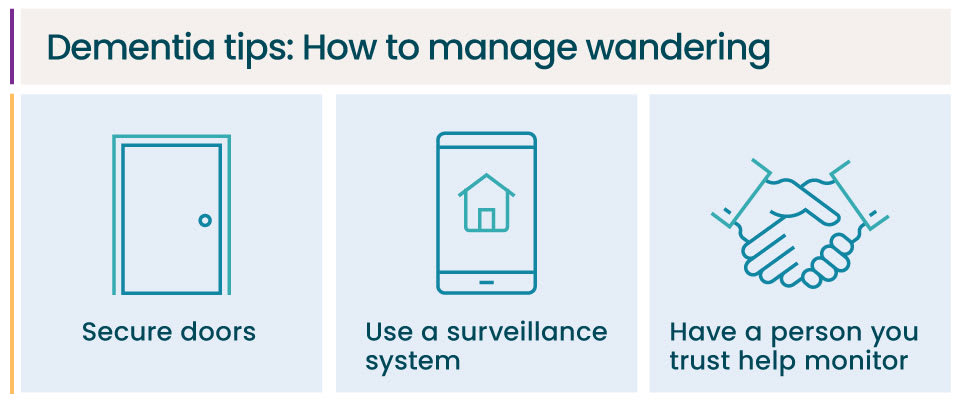
Tips for managing dementia wandering
The No. 1 priority is to keep your loved one safe, Hashmi says. He suggests the following actions:
- Secure all doors. Be especially vigilant about doors that lead outside.
- Use technology. Tracking devices and surveillance systems are widely available and affordable.
- Enlist a team. Neighborhood watch groups and local police are often happy to help keep an eye out for your loved one.

Talk with a Senior Living Advisor
Our advisors help 300,000 families each year find the right senior care for their loved ones.
Remember: Your needs as a caregiver matter too
According to caregiver statistics, caregivers spend nearly all of their excess free time caring for their loved ones. This is even more so the case when caring for someone with dementia. Dealing with dementia behaviors can quickly wear out a caregiver or family member, causing caregiver burnout. Before burnout, it’s helpful to turn to respite care to provide you some relief as you recharge.
However, if your loved one’s dementia behaviors have progressed to the point where you cannot manage them alone, long-term help is also available. Senior care options like home care or memory care can help relieve some of the caregiving burden while also helping to keep your loved one safe.
If you are feeling resentment, anxiety, or depression, seek help. A caregiver support group, counselor, friend, or family member can offer camaraderie and advice.
“Other families, other caregivers, are going through the same thing,” Hashmi says. “They have a lot of common challenges and common solutions to share. And often those are the most effective, because they’re going through exactly the same process.”
A Place for Mom and Cleveland Clinic: Supporting seniors and their families
This article was developed in conversation with Cleveland Clinic Center for Geriatric Medicine Section Chief Dr. Ardeshir Hashmi as part of a series of articles featuring expert advice from Cleveland Clinic geriatricians.
Article updated by A Place for Mom senior copywriter Nirali Desai.
Müller-Spahn, F. (2003, March). Behavioral disturbances in dementia. Dialogues in Clinical Neuroscience.
National Institute on Aging. National Institute of Health. (2017). Alzheimer’s changes in behavior and communication.
Cerejeira, J., Lagarto, L., & Mukaetova-Ladinska, E. B. (2012, May). Behavioral and psychological symptoms of dementia. Frontiers in Neurology.
Khachiyants, N., Trinkle, D., Son, S. J., & Kim, K. Y. (2011, December). Sundown syndrome in persons with dementia: An update. Psychiatry Investigation.
Dettmore, D., Kolanowski, A., & Boustani, M. (2009, February). Aggression in persons with dementia: Use of nursing theory to guide clinical practice. Geriatric Nursing.
Rose, K. M., Fagin, C. M., & Lorenz, R. (2010, May). Sleep disturbances in dementia: What they are and what to do. Journal of Gerontological Nursing.
Agrawal, A. K., Gowda, M., Achary, U., Gowda, G. S., & Harbishettar, V. (2021, September). Approach to management of wandering in dementia: Ethical and legal issue. Indian Journal of Psychological Medicine.
American Psychological Association. (2015). Living well with dementia.
Senior living options in all states
The information contained on this page is for informational purposes only and is not intended to constitute medical, legal or financial advice or create a professional relationship between A Place for Mom and the reader. Always seek the advice of your health care provider, attorney or financial advisor with respect to any particular matter, and do not act or refrain from acting on the basis of anything you have read on this site. Links to third-party websites are only for the convenience of the reader; A Place for Mom does not endorse the contents of the third-party sites.
Make the best senior care decision
Make the best senior care decision